Medication Overuse is Common; Are You at Risk?

As we age, it is a common problem. You may see more than one doctor and each prescribes a different drug for a different illness. Before you know it, you’re taking several medications and start feeling tired, dizzy, or nauseous. This could be interpreted as a new symptom for a new ailment and you are prescribed yet another drug. Before long you are taking a fist full of medications that make you feel even more unwell.
Consider it Canada’s other prescription drug epidemic. For decades, experts have warned that older adults are taking too many unnecessary medications and assigned the term “polypharmacy” to describe when patients are taking 5 or more different medications.

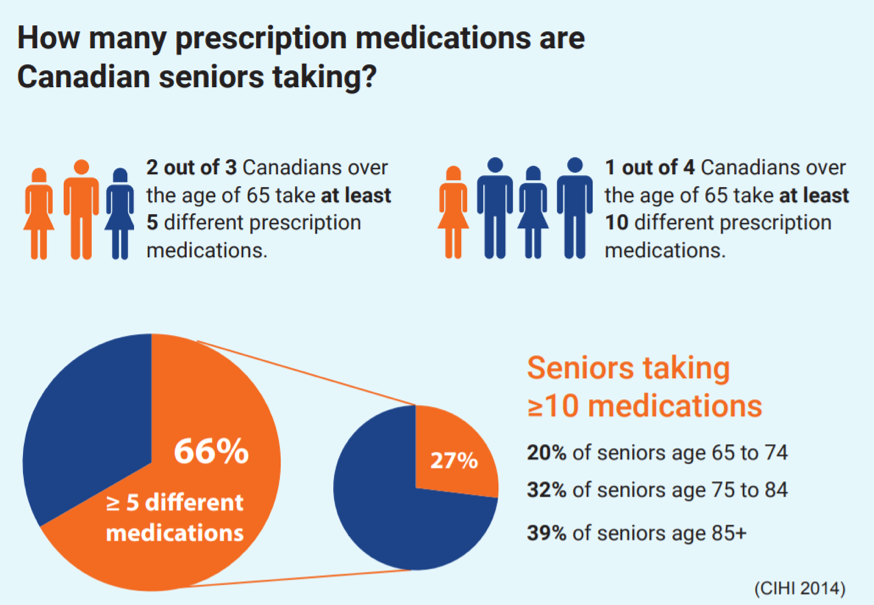
The Problem Of Polypharmacy: Some Scary Stats
In 2016, according to the Canadian Institute for Health Information (CIHI), 2/3 of Canadians aged 65 or older were taking 5 or more prescription medications, 1/4 were taking 10 or more, and 1 in 12 seniors took 15 or more medications.
31.1% of seniors are taking a potentially inappropriate medication (PIM) for older adults on a daily basis. In 2016, a third of all seniors’ hospital visits were due to the use of at least 1 inappropriate medication – a Beers List medication. The Beers List is a 21-page document of medications that are unsafe to be taken in older adults. The take home message here is that there are much safer alternatives to be taken to treat the same conditions.
Why Is Medication Overuse Such A Problem In Older Adults?
Normal aging leads to reductions in many of our vital organ functions. Over time, our liver and our kidneys don’t work as effectively, which causes our bodies to metabolize and eliminate medications less effectively. As a result medications can stick around a lot longer, accumulate in our body and lead to increased side effects. This presents a very important question: If our body is continually changing with age, shouldn’t our doses continually be changing too?
Side Effects Can Be Signs of Medication Overuse
It is important to know that dizziness and drowsiness are not normal processes of aging. Being tired and dizzy all the time suggests that you could be on doses that are too high or you are on too many medications. Dizziness can lead to falls and falls can lead to broken hips, long hospital stays and poor outcomes in older adults.
Other common adverse effects of multiple medications include: Tiredness, sleepiness, decreased alertness, constipation, diarrhea, incontinence, loss of appetite, confusion, falls and other mobility issues, depression, weakness, tremors, hallucinations, anxiety, excitability, sexual dysfunction, skin rashes.
For years healthcare siloing (lack of information exchange amongst healthcare professionals) has been a big problem in the community setting. In the past you would normally have to be admitted into the hospital before you could get great collaborative care. In the hospital doctors can work together with pharmacists, who can assess blood work and get feedback from the nurses to help personalize medications to what your body needs. This process may include lowering a dose, switching to a safer alternative or even deprescribing- the planned process of stopping medications that are no longer necessary. It is not uncommon to hear of patients being admitted into the hospital on 15-20 medications and leave on 5. With so many older adults on 10 or more medications it has left many wondering how did this happen and who is to blame?
This video summarizes polypharmacy and the need to personalize medications to each individual!
Polypharmacy: Who Is To Blame For Medication Overuse?
Drug safety studies usually only enlist younger adults, even if they are for medications that are meant to treat older adults. Clinical Trials often exclude older adults, who often have health conditions or take medications that could “confuse the results of the study”. Problems arise when the safety and max tolerated doses of a young adult are then applied to an older adult, who might have ⅓ to ¼ of the kidney function. A “start low and go slow” mentality is important when starting new medications to help limit the risk of side effects and toxicity. In older adults, often the initial starting dose should be ¼ of the usual adult dose.
Many people are also quick to blame doctors. However, this could not be further from the truth. The problem of polypharmacy is due to lack of healthcare information exchange in the community setting. Doctors and pharmacists both have 4 years of complementary teachings.
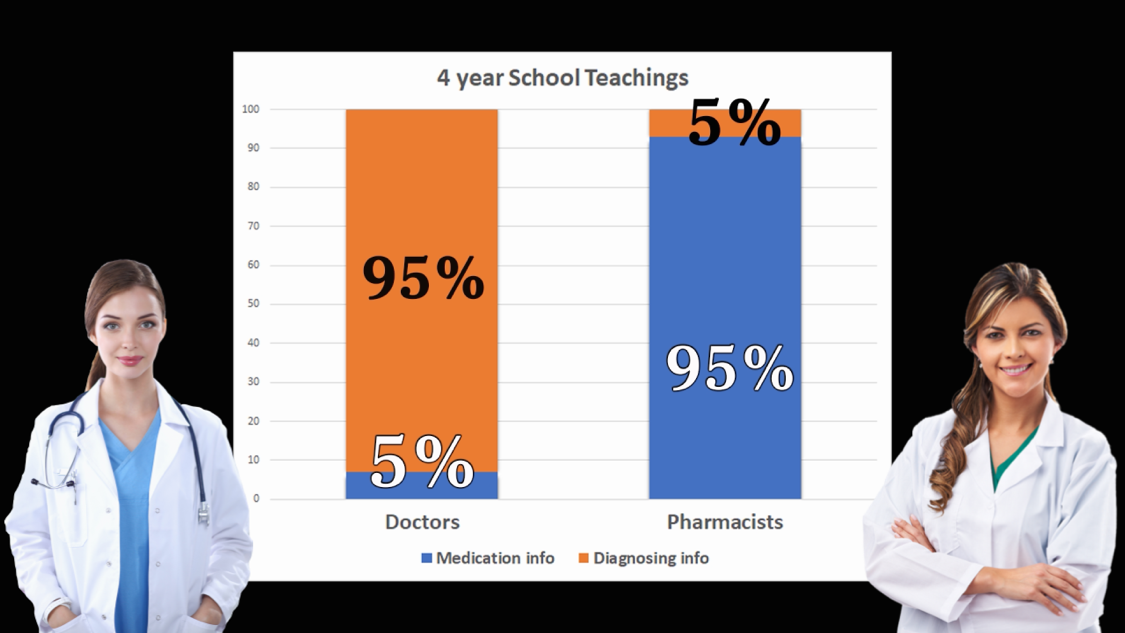
Doctors spend the vast majority of their education on diagnosing and little bit on medications, while pharmacists do the opposite. Yet when they graduate, doctors are responsible for both diagnosing and medication management- which includes selecting medications, adjusting doses and monitoring their safety. In a perfect world, most medication-related tasks would be the responsibility of the pharmacist. It is the system’s fault that has not allowed pharmacists to help out. Until recently pharmacists have not had access to important health information such as diagnoses, health records and lab work. However, it is exciting that WE now do!
e-Health allows pharmacy to help personalize your medications
Electronic health record information systems, like ClinicalConnect, are now allowing for improved information exchange amongst healthcare professionals. The collaborative care model, often seen in the hospital, is now possible in the community setting. Pharmacists and other healthcare professionals are now able to access important information such as diagnoses, doctors reports, and blood work.
Certified Geriatric Pharmacists specialize in how to adapt our medications to our bodies as we age. They can now access blood work to determine your kidney function and how your body processes medication to help assess what might be the right medications and doses for you. With e-Health, the dawn of Clinical Pharmacy is upon us! Clinical Pharmacists are now able to work together with your doctor to help ensure that your medications and doses are right for you.
Want advice about sleep, pain or any other questions about your medications? Contact The Clinical Pharmacy!
Speak with one of The Health Depot’s clinical pharmacists for a FREE no obligation consultation. The Health Depot is changing the face of pharmacy by helping to personalize medications and bring hospital-level collaboration and care into the community setting.
Visit their website to learn more about personalized medications.
CARP Member Benefits:
The Health Depot is the preferred pharmacy of CARP; learn more about member savings and new health services. Visit the CARP member benefits webpage at The Health Depot pharmacy.
The Health Depot’s pharmacists are always accessible and available to speak with you. Call toll free today: 1-855-844-2242

