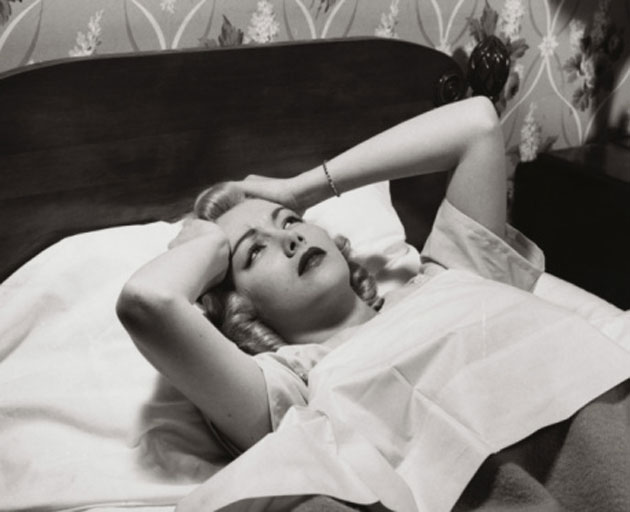
Sleep disorders not only rob us of a myriad of healthy benefits, but at times, they can be downright scary. From sleep paralysis and hallucinations to sexsomnia, we look at some worrisome sleep problems.
Getting a good night’s sleep has been associated with a long list of benefits from lower stress to better heart health, brainpower and longevity.
Sleep disorders not only rob us of these benefits, but at times, they can actually be scary — either because of the health risks they pose or because they are literally frightening.
1. Obstructive Sleep Apnea
Along with insomnia, obstructive sleep apnea is one of the most common sleep disorders, affecting millions of North Americans. “Apnea” — which is Greek for “without breath” — refers to episodes where a person pauses in breathing during sleep. Typically, an episode lasts long enough that one or more breaths are missed, and can occur dozens or even hundreds of times throughout the night.
While sleep apnea occurs in two distinct forms — central and obstructive — obstructive sleep apnea is by far more common. It occurs when soft tissues of the throat relax and cause a physical block to airflow. (In central sleep apnea, the brain doesn’t send the proper signals to the muscles that control breathing.) Symptoms of both varieties overlap, sometimes making a determination between the two difficult.
The scary part? Despite being considered a serious medical condition, sleep apnea often goes undiagnosed. It has been found to increase risk for high blood pressure, heart attack, and stroke. And recently, a pair of studies out of Spain and the US found that sleep apnea can significantly increase risk for cancer. The disorder can also lead to memory problems, mood swings and feelings of depression.
Symptoms include loud snoring, morning headaches and excessive fatigue even after getting a full night’s sleep. Treatments can include sleeping with a CPAP (continuous positive airway pressure) mask, wearing an oral device designed to keep your throat open or in some cases, having surgery to remove excess tissue from your nose or throat.
Other things you can do, according to experts: lose excess weight, avoid alcohol and medications such as tranquilizers and sleeping pills, sleep on your side or abdomen (rather than on your back), and use a saline spray to help keep your nasal passages clear.
2. Sleep Paralysis
Dream activity ramps up during rapid eye movement (REM) sleep, and to keep us from acting out our dreams and possibly harming ourselves, the muscles of the body become immobile. But sometimes this temporary paralysis continues even after a person wakes up.
This inability to move or speak can happen while falling asleep or upon awakening. While the episodes are usually brief, they can be quite frightening. Basically, you know you’re awake — but when you try to move, you can’t. (While experts aren’t sure what causes sleep paralysis, some sources say that people who suffer from it tend to sleep on their back.)
And to make matters worse, sleep paralysis is often accompanied by the next spooky sleep disorder on the list: hallucinations.
3. Sleepy Hallucinations
Like sleep paralysis, these hallucinations (called hypnagogic hallucinations) often occur while falling quickly into REM sleep, as you do when you first fall asleep, or while you’re awaking. And because you’re semi-awake when you begin to dream, these dreams can seem particularly vivid and real.
Typical hallucinations include hearing voices, feeling phantom sensations and seeing people or strange objects in the room. A particularly common vision? Bugs or animals crawling on the wall, experts say. Some researchers even say that reports of alien visitation or abduction could be explained by episodes of sleep paralysis.
As mentioned, many people experience hypnagogic hallucinations and sleep paralysis simultaneously. Taken together, these sleep disorders can be frightening indeed, with many people reporting that they sense an evil presence along with a feeling of being crushed or choked. Such spooky sensations have inspired folklore surrounding the pair of sleep disorders: in Newfoundland, it is called the “Old Hag” and in Mexico it’s known by the idiom “subirse el muerto” — or “the dead climb on top of you”.
Sleep-related hallucinations are also common in people with narcolepsy, another serious sleep disorder. Narcolepsy is associated with excessive daytime sleepiness, involuntary periods of sleep and loss of muscle control.
4. Sleepwalking
It’s more prevalent than you might think. Up to 15 per cent of adults occasionally sleepwalk, experts say. And forget about the notion of sleepwalkers moving slowly around, arms outstretched. Many nighttime wonderers navigate their rooms with ease, even opening doors and moving furniture. (Falling, however, is a very real danger, particularly when stairs are involved.) Another myth: Waking a sleepwalker will not, in fact, do them any harm, despite a common perception this should be avoided.
Experts say that genetics could play a big role, with close relatives of sleepwalkers 10 times more likely to suffer from the disorder than the general population. Stress and disturbed sleep can also play a role.
5. REM Behavior Disorder
This disorder has the opposite affect of sleep paralysis. Instead of experiencing too much immobility, a person with REM Behavior Disorder has too little of it. When this happens, people act out their dreams, which can be harmful to themselves or others if the dream happens to be violent. Examples include yelling, punching, kicking, and even getting out of bed and running around. After awakening, a person may remember their dream, but not speaking or moving.
This particular disorder occurs most often among older adults, and it can be a symptom of Parkinson’s disease. It can be treated with medications that reduce REM sleep and relax the body.
6. Nocturnal Sleep-Related Eating Disorder
This disorder is a dieter’s nightmare, literally. People with a sleep-related eating problem go on nocturnal eating binges — and often don’t even remember it the next morning. Even worse: they can injure themselves by chopping ingredients, burning themselves on the oven or serving up unhealthy and unsavory dishes like raw or frozen food.
Not much is known about this sleep disorder, but like sleepwalking, it occurs during non-REM sleep. Experts say that certain drugs that increase dopamine, a neurotransmitter associated with reward and pleasure, can help stop the unconscious nighttime noshing.
7. Sexsomnia
If you think eating in your sleep is strange, how about having sleep sex? Sexsomnia, first described in a 1996 case study of seven individuals, can include symptoms ranging from the annoying (loud moaning) to the dangerous (self-injurious masturbation) to the criminal (sexual assault or rape). In several recent controversial cases, men have been acquitted of sexual assault by arguing that they were asleep during the attack.
While research on sexsomnia is limited, some experts suggest that factors such as sleep deprivation, stress, alcohol, drugs and physical contact with a bed partner could play a role.
8. Night Terrors
Unlike nightmares, night terrors are technically not dreams, but a strong reaction as a person transitions from one sleep phase to another. This disorder, which can cause intense fear, is most common among children and usually occurs two to three hours after sleep begins.
A person experiencing a night terror may suddenly sit up with their eyes open, although they usually aren’t actually seeing what is in front of them. Yelling, screaming, and thrashing are common, and in some cases, night terrors mix with sleepwalking. Although it is difficult to comfort, or even awaken, a person in the midst of a terror, the episode generally passes within 10 to 15 minutes.
Like many other sleep disorders, the cause remains a mystery, although some experts point to triggers such as fever, irregular sleep and stress. The good news for children (and their parents) experiencing this disorder is that it is usually outgrown.
What can you do?
If you’re experiencing sleep problems on an ongoing basis, it’s important to consult with your doctor who may refer you to a sleep clinic for diagnosis. This often involves spending a night or two in a sleep lab, where heart, brain, movements and breathing patterns can be monitored during sleep. Treatments can vary from medical interventions and drugs to lifestyle changes that can improve sleep hygiene.
Sources: Mayo Clinic, American Sleep Association, WebMD, National Institutes of Health, Centers for Disease Control and Prevention, LiveScience, Science2.0, EverydayHealth.com, CTV
A version of this story was published online on March 1, 2019
RELATED:
When Sleep Evades You, Cognitive Behavioural Therapy Might Help